The MediSked Blog
Preventing Fraud with Human Services Software
Posted by Mike Holihan on Thu, Dec 27, 2012 @ 10:14 AM
News recently broke in Virginia of a human service agency employee that was sentenced to ten months in prison for altering client records in order to cover up Medicaid fraud. You can find the article here. Over a three year period, under the direction of the owner, the agency billed for and received reimbursements for 900 fake claims for providing respite services to 30 clients. In total, the agency received over $630,000 of fraudulent Medicaid money. Staff were told to falsify and make false entries to time sheets and office records to make it seem as though respite service had occured when, indeed it had not. Ultimately, the case was investigated at the highest level - the FBI - and the Virginia State Attorney General's Office. The employee has been charged with health care fraud, alteration of records and aggravated identity theft.
Tags: Compliance, Provider Agencies, Medicaid
Know the Center for Program Integrity goals from CMS.gov
Posted by Mike Holihan on Tue, Nov 20, 2012 @ 02:59 PM
Tags: Compliance, CMS
OIG Update; Audit of Personal Care Services in West Virginia
Posted by Mike Holihan on Wed, Oct 17, 2012 @ 05:06 PM
In total, the audit report recommends that the State agency:
- Refund $360,539 to the Federal Government and
- Improve its monitoring of providers to ensure compliance with Federal and State requirements for personal care services.
To view the full report, click here.
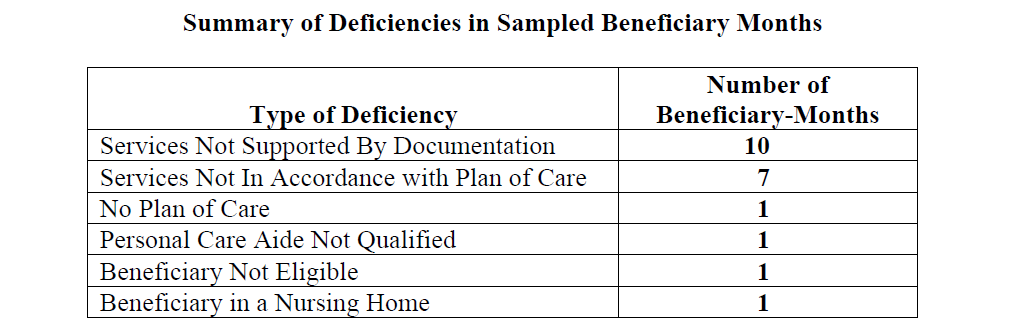
The two main deficiencies laid out in this report are Services Not Supported by Documentation and Services Not In Accordance with Plan of Care.? If agencies are still utilizing paper based methods to document services and plans of care, they run a real risk of incurring these types of deficiencies.
Everyone knows that auditors are looking very carefully for misuse of Medicaid dollars.? Human error is a fact of life when agencies put their faith in paper, binders and non-electronic sources.
For a free report on the most common audit issues for home health and human service provider agencies, click here.? Agencies Management Platforms, such as MediSked Connect, remove human error and eliminate the common audit issues, including the deficiencies listed in this report.
Tags: Compliance, Medicaid, Waiver Services