In total, the audit report recommends that the State agency:
- Refund $360,539 to the Federal Government and
- Improve its monitoring of providers to ensure compliance with Federal and State requirements for personal care services.
To view the full report, click here.
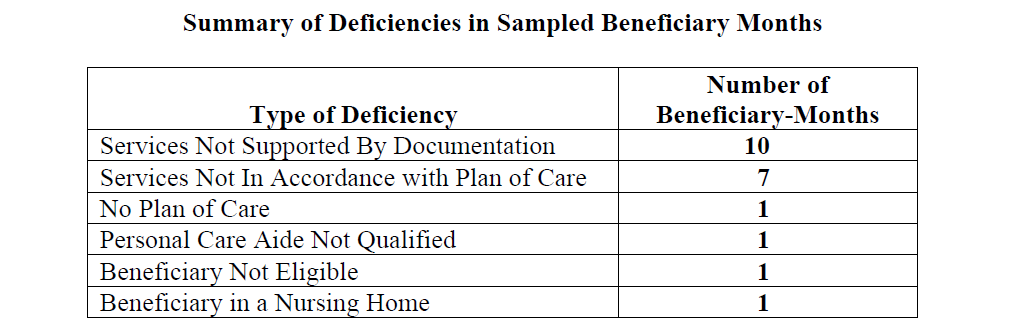
The two main deficiencies laid out in this report are Services Not Supported by Documentation and Services Not In Accordance with Plan of Care.? If agencies are still utilizing paper based methods to document services and plans of care, they run a real risk of incurring these types of deficiencies.
Everyone knows that auditors are looking very carefully for misuse of Medicaid dollars.? Human error is a fact of life when agencies put their faith in paper, binders and non-electronic sources.
For a free report on the most common audit issues for home health and human service provider agencies, click here.? Agencies Management Platforms, such as MediSked Connect, remove human error and eliminate the common audit issues, including the deficiencies listed in this report.